Cervical cancer is a cancer that has plagued women for a long time, with more than 500,000 new cervical cancers worldwide every year and more than 300,000 deaths per year. The prevention and treatment situation of cervical cancer in China is grim, and the incidence of cervical cancer continues to increase and shows a trend of younger people [1]. In November 2020, the World Health Organization launched the Global Strategy to Accelerate the Elimination of Cervical Cancer, the first global commitment to eliminate a cancer. In 2023, China's National Health Commission, the Ministry of Education and other 10 departments have jointly issued the Action Plan to accelerate the elimination of Cervical cancer (2022-2030), aiming to establish a multi-sectoral comprehensive prevention and control mechanism for cervical cancer, accelerate the elimination process of cervical cancer in China, and protect and promote the health of women.
Early screening and timely intervention are crucial for the prevention and treatment of cervical cancer. The current cervical cancer screening mainly relies on high-risk HPV detection and ThinPrep cytologic test (TCT). The World Health Organization (WHO) and the United Nations Special Programme for Human Reproduction (HRP) released the second edition of the Cervical Precancerous Screening and Treatment Guidelines on July 6, 2021, using HPV DNA testing as a primary screening method for cervical cancer. However, more than 85% of women will be infected with HPV in their lifetime, and the vast majority of HPV will be cleared by the body's immune system within 2 years, resulting in a large number of unnecessary colposcopic referrals and excessive anxiety.
On February 5, 2024, China Welfare Society International Peace Maternal and Child Health Hospital (Shanghai Jiao Tong University School of Medicine affiliated International Peace Maternal and Child Health Hospital) Professor Wang Yudong's team and Fudan University Institute of Biomedical Research Professor Yu Wenqiang's team published in the international journal BMC Medicine (IF=11.8) entitled "PCDHGB7 hypermethylation based Cervical cancer Methylation (CerMe) detection for the triage of high-risk human papillomavirus positive women: A prospective cohort study (Figure 1a). The study validated a large clinical sample of more than 3,000 patients and found that PCDHGB7 gene methylation testing has great advantages and outstanding clinical performance as a shred in HPV-positive patients. Compared with TCT, PCDHGB7 gene methylation assay (CerMe) showed better sensitivity, specificity, positive predictive value and negative predictive value. As an accurate, efficient, convenient, fast and empirical detection method, this technology can effectively reduce the missed diagnosis and misdiagnosis of cervical cancer caused by the difference in pathological diagnosis level between developed and poor areas.
Pic 1a
A large cohort study of prospective screening to propose a new strategy for non-invasive shunt testing of HRHPV-positive patients
High-risk human papillomavirus (hrHPV) detection is the first recommended cervical cancer screening method in domestic and foreign guidelines, which has greatly reduced the incidence and mortality of cervical cancer. However, most hrHPV infections are transient, resulting in a large number of HRHPV-positive patients receiving unnecessary colposcopic referrals. As the most commonly used shunt strategy, cytology is less sensitive and affected by subjective factors. Therefore, the development of an efficient, non-invasive and objective shunt method to reduce the over-referral of HRHPV-positive patients is an urgent need for accurate prevention and treatment of cervical cancer.
The study established a prospective cohort of 3251 HRHPV-positive women and took the remaining samples of cervical exuded cells for testing PCDHGB7 methylation to develop a CerMe test that can effectively distinguish between cervical intraepithelial neoplasia grade 1 and below (CIN1-) and CIN2 and above (CIN2+). The sensitivity was 82.4% and the specificity was 91.1%. Compared with cytology, CerMe reduced the number of referrals for non-16/18 HRHPV-positive women by 62.2% (383/616) and showed superior specificity (92.0% vs. 74.9%). Among hrHPV16/18 positive women, CerMe testing reduced referrals by 26.0% (77/296) and showed significantly increased sensitivity (80.7% vs. 61.5%) and specificity (88.5% vs. 75.3%). CerMe also performed well as a shunt strategy in HRHPV-positive patients with cytology as ASC-US or LSIL. In addition, CerMe semi-quantitative stratification analysis can be used as a reference index for colposcopy and pathological biopsy, and its combined detection with cytological stratification (MeCy) can prevent the missed diagnosis of CIN2+ to a certain extent, especially the missed diagnosis of cervical adenocarcinoma with hidden lesions. Follow-up studies will explore the predictive value of CerMe testing for disease progression through follow-up of high-risk patients.
The whole cancer marker target has been developed over time, and the detection of PCDHGB7 methylation is endless
As the basis for the preliminary work of this study, as early as June 2021, The team published a paper entitled "Hypermethylated PCDHGB7 as a universal cancer only" in the International Journal of Clinical and Translational Medicine (2020 IF=11.492) The paper "marker and its application in early cervical cancer screening" (FIG. 1b) for the first time demonstrated the discovery process of "whole cancer marker" PCDHGB7 and its important significance for cancer research and early cervical cancer screening. Total cancer markers are common markers of a series of tumors. Currently, the published total cancer markers include HIST1H4F, PCDHGB7 and SIX6[2-4]. Researchers have verified the possibility of PCDHGB7 gene methylation detection as a means of cervical cancer screening in samples of cervical tissue and exuded cytology and vaginal secretions, and determined that PCDHGB7 can be used as a marker for early diagnosis of cervical cancer, but there is a lack of clinical validation in large samples.
Pic 1b
PCDHGB7 gene methylation detection, accurately shunt high-risk hrHPV population
In the newly published study [5], the researchers validated the efficacy of PCDHGB7 gene methylation in detecting cervical cancer in a large clinical cohort. We collected cervical cell samples from 3251 HRHPV-positive women aged 30-82 years (Figure 2) to establish a cervical cancer PCDHGB7 gene methylation detection model (CerMe) to evaluate CerMe's performance as a triage for HRHPV-positive population. CerMe demonstrated an effective ability to distinguish cervical cancer CIN1 from CIN2+ (Figure 3) and demonstrated excellent specificity (91.1% vs. 77.9%) and sensitivity (82.4% vs. 65.9%) when compared to cytological triage efficacy (Figure 4). Considering the imbalance in the distribution of medical resources among regions in China and the serious shortage of personnel in pathological diagnosis in primary hospitals, CerMe, as a de-empirical, convenient and fast detection means, brings a new solution for cervical cancer screening and diagnosis and treatment.
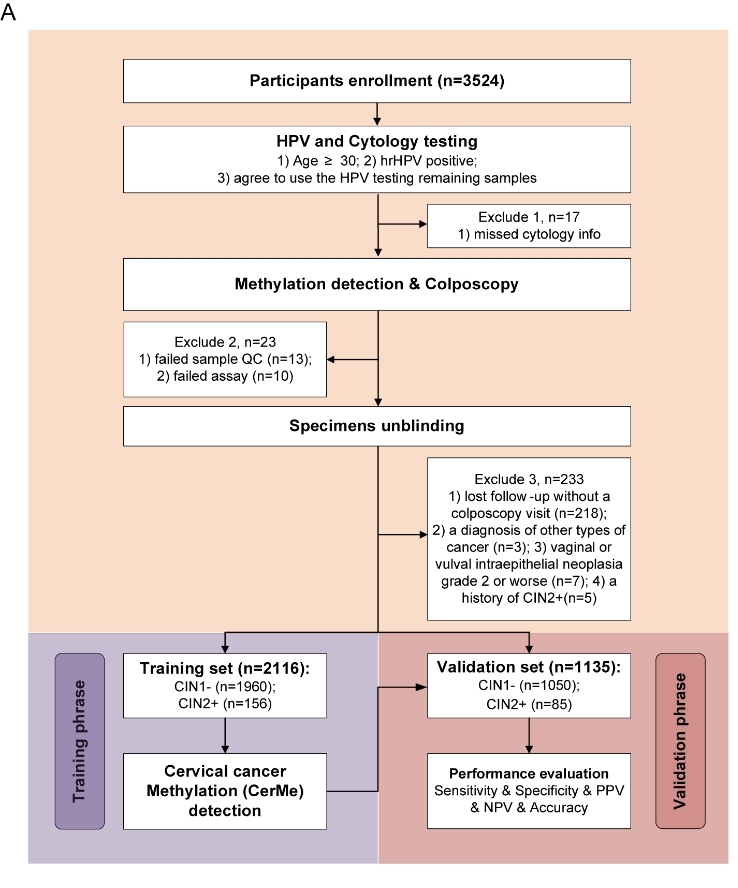
Pic2 Flow chart of clinical studies for CerMe testing
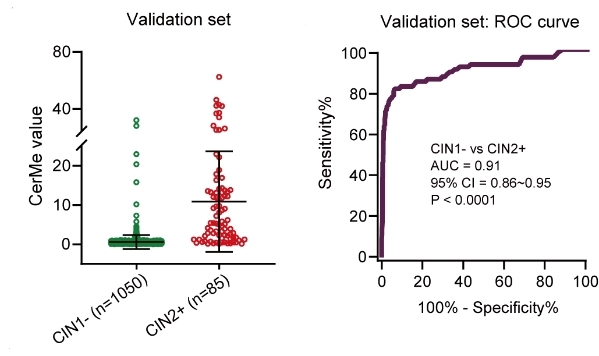
Pic3 The CerMe test can effectively distinguish cervical precancerous lesions
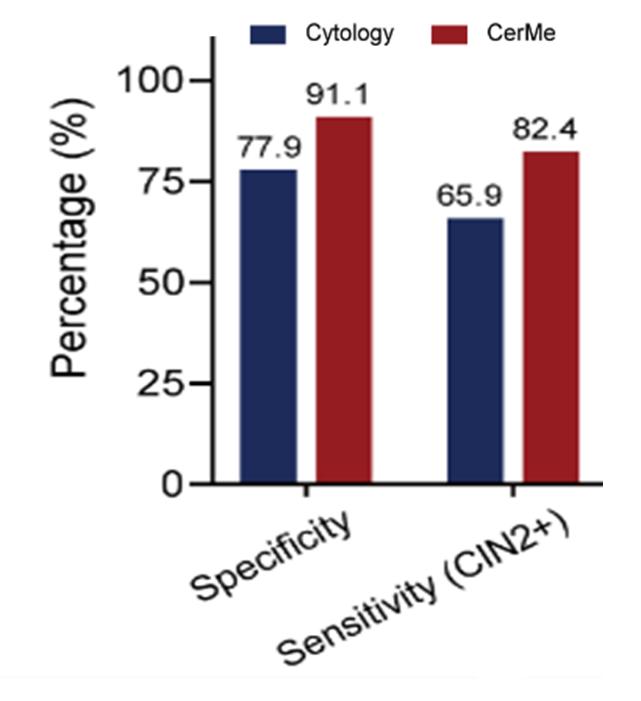
Pic4 CerMe test has better triage ability for HRHPV-positive population than cytology
Standardized diagnosis and treatment! CerMe testing effectively reduces colposcopic referrals
Women who are positive for hrHPV16/18 during routine cervical cancer screening are often recommended to be referred directly to colposcopy; Other women with type 12 HRHPV-positive are recommended to undergo cervical exfoliation cytology and then refer to colposcopy when the test results are ≥ASCUS. The overall HPV infection rate in the general female population aged 20 years and above in China is 15.0%[6], and excessive colposcopic referrals increase the social and economic burden. The researchers further analyzed the triage efficacy of CerMe in women with different subtypes of hrHPV infection, and in women with other 12 HRHPV-positive types, CerMe test reduced the referral rate by 62.2%, showing superior specificity (92.0% vs. 74.9%). Among HPV16/18 positive women, the CerMe specificity was 88.5%. Overall, CerMe testing provides an optimal triage strategy for HRHPV-positive women to reduce over-referral for colposcopy, especially in areas with strained health care resources.
Clear the fog to see the truth! The CerMe test truly assesses the risk of cervical cancer
HPV typing and cytology tests make it difficult to assess a woman's true risk of cancer. Can CerMe test answer this question? The study calculated the proportion of colposcopy (normal, CIN1, CIN2/3, cancer) in CerMe stratification results, with CerMe NPV up to 98.1% and CerMe strongly positive PPV up to 90.6% (NPV= true negative population/test negative population) in people with normal colposcopy. PPV= true positive population/test positive population) (Figure 5), suggesting a higher risk of cancer in strongly positive CerMe patients. At the same time, we further compared the proportion of CerMe positive in colposcopy results, and we also observed that the proportion of positive CerMe gradually increased with disease progression (normal: 7.5%; CIN1:16.7%; CIN2/3: 74.4%; Cervical cancer: 97.6%). We have proved from both positive and negative aspects that CerMe can assess the real disease risk. The real risk of CerMe strongly positive patients is extremely high, which deserves further clinical attention, and helps to eliminate the anxiety and worry of HPV-positive patients. Through CerMe test, we can know well and do not panic.
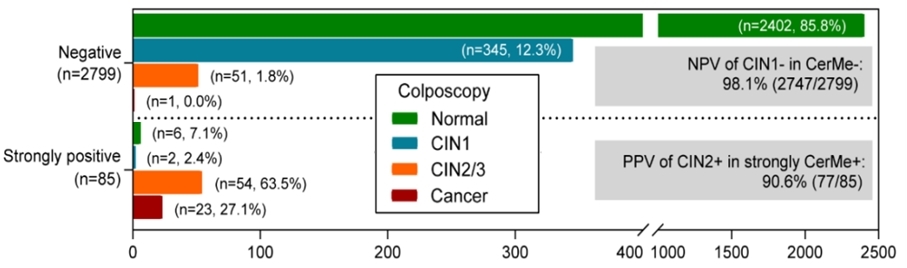
Pic5 The higher the CerMe value, the higher the risk of disease
There is no disguise to hide! The CerMe test is effective in reducing missed diagnosis of cervical adenocarcinoma
Adenocarcinoma of the cervix originates from columnar epithelial cells (single layer) in the cervical canal, the location of the disease is relatively hidden, and the positive signs of gynecology are not obvious. About 15% of cervical adenocarcinomas are not associated with HPV infection, so these cases are not sensitive to existing screening methods. The researchers compared CerMe with cytological tests for cervical squamous cell carcinoma (SCC) and cervical adenocarcinoma (AC) in HRHPV-positive women. The results showed that CerMe performed better than cytological tests for cervical adenocarcinoma (90% vs. 60%) and cervical squamous cell carcinoma (100% vs. 78.1%) (Figure 6). CerMe test can effectively make up for the defects of conventional cervical cancer screening methods for cervical adenocarcinoma.
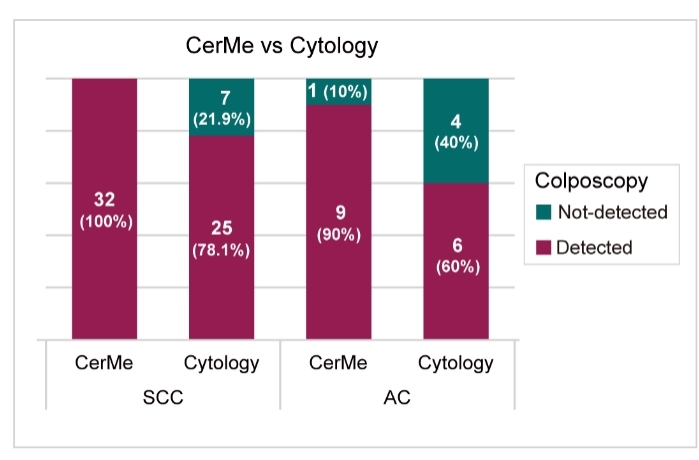
Pic6 CerMe test can effectively prevent the missed diagnosis of cervical adenocarcinoma
Total cancer markers are associated with a large real-world cohort, reducing overdiagnosis and effectively avoiding missed diagnosis and misdiagnosis.
This prospective study, based on high-risk HPV-positive women, reveals that the CerMe test is a highly effective molecular test independent of the pathologist's subjective experience and can reflect the true risk of cervical cancer. The test can directly use HPV DNA to detect samples without re-sampling, minimizing the burden on patients and physicians; It can effectively reduce unnecessary colposcopy in the most common ASC-US and LSIL cytological populations in screening programs and some HRHPV-positive patients with non-persistent infections, avoiding over-diagnosis and treatment.
A new chapter in common spectrum diagnosis and treatment! Total cancer markers help open the new door of accurate prevention and treatment of cervical cancer
The study was conducted by Professor Wang Yudong, International Peace Maternal and Child Health Care Hospital, Shanghai Jiao Tong University School of Medicine, and Professor Yu Wenqiang, Institute of Biomedical Research, Shanghai Medical College, Fudan University. Dr. Cao Dan, Cervical Department, International Peace Maternal and Child Health Hospital, Shanghai Jiao Tong University School of Medicine, and Dr. Yang Zhicong, Institute of Biomedical Sciences, Fudan University, are co-first authors of this paper. This research was supported by the Shanghai Science and Technology Commission and the Shanghai Municipal Health Commission.
Since it was approved as the Cervical Disease Diagnosis and Treatment Center of Shanghai Jiao Tong University School of Medicine in 2019, the National Department of Gynecology and Infantile Cervix has established a comprehensive and standardized screening, diagnosis and follow-up system for cervical cancer and precancerous lesions, which is in a leading position in the Yangtze River Delta and even the whole country. Wu Dan, Director of the Cervical Department, and his team have accumulated rich clinical experience in the diagnosis and treatment of cervical cancer and precancerous lesions, and have made a number of scientific breakthroughs. In the past 20 years, Wang Yudong led the team to always devote to the treatment of gynecological tumors, the annual operation volume of more than 1000 cases. He innovatively put forward the minimally invasive surgery for cervical cancer - "playing a karez" and was widely used in clinical treatment, significantly improving the surgical treatment effect of cervical cancer. In addition, Wang Yudong and his team based on the clinical treatment and basic research of pregnancy complicated with gynecological malignant tumors, advocated the multidisciplinary combined treatment of gynecological tumors, and accumulated rich experience and made many breakthroughs in pregnancy complicated with malignant tumors and the preservation of fertility in patients with malignant tumors. Since 2015, Wang Yudong's team has conducted cervical lesions examination on community-age women, followed up 1,000 patients with official neck lesions, conducted integrated analysis of clinical information, pathological information and biological information of patients with lesions, and assessed the correlation between various risk factors and disease progression. In addition, Wang Yudong's team also carried out research on early cervical cancer screening based on artificial intelligence. They applied artificial intelligence technology to cervical cytology screening to develop a deep learning-based cervical cancer screening model. In recent years, the research of Wang Yudong's team on the early detection of cervical cancer has focused on the relationship between DNA methylation and the occurrence and development of cervical cancer, and verified that PCDHGB7 gene methylation detection can be used as a means of cervical cancer screening and early detection, and can effectively make up for the shortcomings of existing cytology and high-risk HPV detection technology.
Professor Yu Wenqiang's team has been working in the field of DNA methylation for more than 20 years, during which time it has developed a new whole-genome DNA methylation detection method with independent intellectual property rights, GPS (Guide Positioning Sequencing), that is, "guided positioning sequencing". The sequencing technology broke through the bottleneck of low comparison rate of WGBS technology, GPS technology increased the detection coverage of CpG island to 96%, and drew the world's first single base accuracy of the whole genome DNA methylation map, GPS technology greatly improved the accuracy of DNA methylation sequencing. Based on GPS technology for high-precision and high-coverage methylation detection of whole genome DNA, Professor Yu Wenqiang's team found a class of methylation sites common in tumors, and proposed the concept of "Universal Cancer Only Marker" (UCOM) for the first time in the world. This led to the discovery of a range of TAGMe® whole-cancer tumor markers. As of January 2024, these whole cancer tumor markers have been double-blind validated in more than 90,000 clinical samples, with an overall compliance rate of 90% in tissue samples.
Reference List
1.Siegel Rebecca L,Miller Kimberly D,Wagle Nikita Sandeep et al. Cancer statistics, 2023.[J] .CA Cancer J Clin, 2023, 73: 17-48.
2.Dong Shihua,Lu Qi,Xu Peng et al. Hypermethylated PCDHGB7 as a universal cancer only marker and its application in early cervical cancer screening.[J] .Clin Transl Med, 2021, 11: e457.
3.Dong Shihua,Yang Zhicong,Xu Peng et al. Mutually exclusive epigenetic modification on SIX6 with hypermethylation for precancerous stage and metastasis emergence tracing.[J] .Signal Transduct Target Ther, 2022, 7: 208.
4.Dong Shihua,Li Wei,Wang Lin et al. HIST1H4FHistone-Related Genes Are Hypermethylated in Lung Cancer and Hypermethylated Could Serve as a Pan-Cancer Biomarker.[J] .Cancer Res, 2019, 79: 6101-6112.
5. Cao D, Yang Z, Dong S, Li Y, Mao Z, Lu Q, et al. PCDHGB7 hypermethylation-based Cervical cancer Methylation (CerMe) detection for the triage of high-risk human papillomavirus-positive women: a prospective cohort study. BMC Medicine. 2024;22:55.
6.BAO H L, JIN C, WANG S, et al. Prevalence of cervicovaginal human papillomavirus infection and genotypes in the prevaccine era in China: A nationwide population-based study[J]. J Infect, 2021, 82(4):75-83.
Post time: Apr-11-2024

